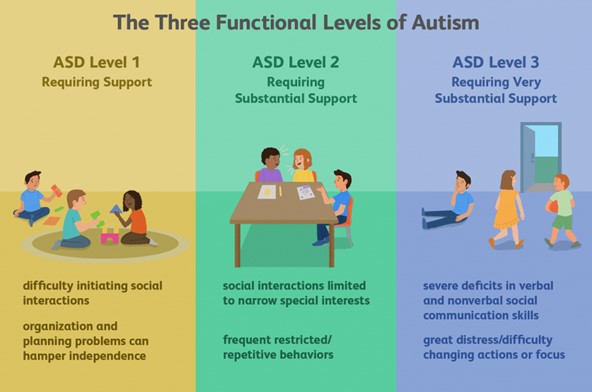
Comprehensive Nutritional and Dietary Intervention for Autism Spectrum Disorder—A Randomized, Controlled 12-Month Trial
This study involved a randomized, controlled, single-blind 12-month treatment study of a comprehensive nutritional and dietary intervention. Participants were 67 children and adults with autism spectrum disorder (ASD) ages 3–58 years from Arizona and 50 non-sibling neurotypical controls of similar age and gender. Treatment began with a special vitamin/mineral supplement, and additional treatments were added sequentially, including essential fatty acids, Epsom salt baths, carnitine, digestive enzymes, and a healthy gluten-free, casein-free, soy-free (HGCSF) diet. There was a significant improvement in nonverbal intellectual ability in the treatment group compared to the non-treatment group (+6.7 ± 11 IQ points vs. −0.6 ± 11 IQ points, p = 0.009) based on a blinded clinical assessment. Based on semi-blinded assessment, the treatment group, compared to the non-treatment group, had significantly greater improvement in autism symptoms and developmental age. The treatment group had significantly greater increases in EPA, DHA, carnitine, and vitamins A, B2, B5, B6, B12, folic acid, and Coenzyme Q10. The positive results of this study suggest that a comprehensive nutritional and dietary intervention is effective at improving nutritional status, non-verbal IQ, autism symptoms, and other symptoms in most individuals with ASD. Parents reported that the vitamin/mineral supplements, essential fatty acids, and HGCSF diet were the most beneficial.
1. Introduction
Many studies have demonstrated that children and adults with ASD often have significant nutritional deficiencies, metabolic imbalances, and digestive problems. Several nutritional and dietary treatment studies have demonstrated benefits in treating these underlying conditions [1,2,3]. In the following sections we discuss specific research related to vitamins, minerals, essential fatty acids, mitochondrial disorders/carnitine issues, and gastrointestinal disorders (digestive problems and food sensitivities).
1.1. Vitamins/Minerals
Several studies suggest that customized vitamin/mineral supplementation is beneficial for children with ASD. Three studies have demonstrated that children with ASD have impaired methylation, decreased glutathione, and increased oxidative stress [4,5,6]. Those studies demonstrated that nutritional supplementation (with methyl-B12, folinic acid, and trimethylglycine) is beneficial. Several other studies have also demonstrated increased oxidative stress [7,8,9,10,11,12]. Methylation is important because that controls epigenetics, and there is evidence that there are many differentially methylated regions in the brains of children with ASD vs. controls [13].
In 2008/2009 we conducted an extensive comparison of the nutritional and metabolic status of children with ASD (n = 55) compared to neurotypical children of similar age and gender (n = 44) [14]. Study measurements included vitamins, biomarkers of vitamin status, minerals, plasma amino acids, plasma glutathione, neurotransmitters, and biomarkers of oxidative stress, methylation, sulfation and energy production. Many statistically significant differences (p < 0.001) were observed in the ASD group compared to the neurotypical group, including: low levels of biotin, glutathione, methylation status (S-adenosylmethionine (SAM) and uridine), ATP, NADH, NADPH, sulfate (free and total), tryptophan, and GABA; also, high levels of oxidative stress markers and plasma glutamate.
That study was followed by a three-month randomized, double-blind, placebo-controlled treatment study involving a customized vitamin/mineral supplement [15]. The supplement was found to be well-absorbed and result in many significant improvements in metabolic status, including SAM, reduced glutathione, ratio of oxidized glutathione to reduced glutathione (GSSG:GSH), nitrotyrosine, ATP, NADH, and NADPH. Most of these metabolic biomarkers improved to normal or near-normal levels. However, although free and total plasma sulfate levels improved, they remained below normal, suggesting that additional treatments are needed to fully normalize sulfation. That study also found that the supplement group had significantly greater improvements than the placebo group on autism-related symptoms on the Parental Global Impressions-Revised Average Change (p = 0.008), and on the subscores for Hyperactivity (p = 0.003), Tantrumming (p = 0.009), Overall (p = 0.02), and Receptive Language (p = 0.03).
1.2. Essential Fatty Acids
Several polyunsaturated fatty acids (PUFAs) are either essential or conditionally essential, including several omega-3 and omega-6 fatty acids. Meta-analyses of many studies have demonstrated that omega-3 levels are decreased in certain psychiatric disorders including schizophrenia (meta-analysis of 14 studies) [16], ADHD (9 studies) [17]), depression (14 studies) [18], bipolar disorder (six studies) [19], and dementia (10 studies) [20].
Meta-analyses of many clinical trials have demonstrated benefits of supplementation with omega-3 PUFA’s for schizophrenia (10 trials) [21], ADHD (16 trials) [17], major depression (12 trials) [22], bipolar depression (5 trials) [23], and possibly dementia (eight of 13 trials positive) [24]. Meta-analyses findings indicated that EPA was more beneficial than DHA, and that higher levels of EPA were more beneficial. There is also one study [25] that found omega-3 fatty acid supplementation is very helpful for infants with Rett’s syndrome, a disorder which often includes autistic symptoms.
PUFA’s may also play a role in some gastrointestinal problems, since they are important for intestinal membrane function. One epidemiological study found that increasing incidence of Crohn’s disease correlated very strongly (r = 0.79) with low levels of omega-3 fatty acids [26]. A one-year, double-blind, placebo-controlled trial of fish oil (2.7 g/day of omega-3 fatty acids) in people with Crohn’s disease found that subjects taking the fish oil had a significantly reduced relapse rate, with no significant adverse effects [27]. Gastrointestinal problems are common in ASD [14,28], and PUFA supplementation may be beneficial for reducing some gastrointestinal problems in children with ASD.
A meta-analysis [29] of fifteen case-control studies (n = 1193) found that, compared with typically developed individuals, the ASD group had lower eicosapentaenoic acid (EPA), docosahexaenoic acid (DHA) and arachidonic acid (AA), and a lower ratio of total omega-3 to total omega-6 fatty acids; these differences were primarily found in studies with children, and not in studies with adolescents or adults. A meta-analysis [29] of four small randomized controlled trials (n = 107) [30,31,32,33] found that compared with placebo, omega-3 fatty acid supplementation improved social withdrawal (p < 0.02) and restricted interests and behaviors (p = 0.05), but did not have a significant effect on communication, irritability, or hyperactivity (all rated per the Aberrant Behavior Checklist). These studies only lasted 6–16 weeks, so were too short to observe full effect, since omega-3 supplementation requires about six months to reach steady-state levels in erythrocytes, and about 1–1.5 months for half of that change to occur [34]. These studies used doses of 0.5–1.5 g/day of omega-3 fatty acids. Two other small randomized studies [35,36] not included in the meta-analysis [29] did not find significant effects on symptoms despite longer duration (6 months), possibly due to small sizes (under 35 participants completed each study) or low dose (200 mg DHA) in one study [36].
Overall, it appears that omega-3 fatty acids are decreased in ASD, and that supplementation may be helpful. Higher doses and longer treatment may result in greater benefit. For example, a treatment study for Crohn’s disease found that long-term treatment (12 months) may be needed for improvement in gastrointestinal problems. We hypothesize that children with ASD who do not regularly eat seafood (the major source of omega-3 fatty acids in most western diets) are more likely to benefit from fish oil supplementation.
1.3. Sulfate
Sulfur is the fourth most common mineral in the body [37]. Most sulfate is produced in vivo by metabolism of cysteine [14]. Sulfation is important for many reactions including detoxification, inactivation of catecholamines, synthesis of brain tissue, sulfation of mucin proteins which line the gastrointestinal tract, and more. Low free and total plasma sulfate in children with ASD has been previously reported in three studies [14,38,39], and is consistent with four studies [38,40,41,42] which found that children with ASD, compared to controls, had a significantly decreased sulfation capacity, based on decreased ability to detoxify paracetamol (acetaminophen). The finding of low plasma sulfate is also consistent with a large study that found high sulfate in the urine of children with ASD [43], as sulfate wasting in the urine partly explains low levels in the plasma. ATP is required for the kidneys to resorb sulfate, and one study [14] found that plasma ATP was low in children with ASD and moderately correlated with levels of free and total plasma sulfate (r = 0.32 and 0.44, respectively), suggesting, that low levels of ATP are a contributor to decreased sulfate in children with ASD. One study [43], also reported high levels of urinary sulfite in children with ASD, suggesting that there was a problem of converting sulfite to sulfate in the mitochondria. In 38% of cases (14/38) urinary sulfite and sulfate levels improved by giving 50 mcg of molybdenum, based upon molybdenum dependence of the enzyme necessary for converting sulfite to sulfate (sulfite oxidase). Another study [15] found that a vitamin/mineral supplement (containing molybdenum) was able to improve, but not normalize, free and total plasma sulfate in children with ASD. Overall, these studies suggest that sulfate is low in children with ASD, and that vitamin/mineral supplementation is helpful but additional sources of sulfate (such as Epsom salt baths) are needed.
1.4. Carnitine and Mitochondrial Disorders
Carnitine is a conditionally essential nutrient that is vital in energy production and fatty acid metabolism. Carnitine carries long-chain fatty acids (fuel) into the mitochondria, and it also carries potentially toxic organic acids out of the mitochondria and cell so they can be eliminated from the body. Several studies have suggested that mitochondrial disorders are common in children with ASD [44,45,46,47,48]. Note that the term “mitochondrial disorders” is used to denote a generalized impairment of mitochondrial function, and are generally not as severe as “mitochondrial diseases”, which involve specific severe genetic abnormalities. One study found decreased levels of carnitine in children with ASD [49]. A recent double-blind, placebo-controlled 3-month study (n = 30) found that supplementation with carnitine was beneficial [50]. Specifically, the study found significantly greater improvements in the Childhood Autism Rating Scale 2 (CARS-2) and Clinical Global Impressions (CGI) scores in the treatment group compared to the placebo group. In addition, scores significantly improved in cognition and marginally in speech on the Autism Treatment Evaluation Checklist (ATEC). l-carnitine therapy significantly increased serum carnitine concentrations, and significant correlations between changes in serum free-carnitine levels and positive clinical changes were observed. l-carnitine therapy was generally well-tolerated by study subjects. A second study [51] found similar results.
Overall, the literature suggests that mitochondrial disorders are common in ASD, and that a combination of therapy with vitamins, minerals, CoEnzyme Q10, essential fatty acids, and l-carnitine may be helpful in improving mitochondrial function.
1.5. Gastrointestinal Problems, Digestive Enzymes, Limited Diets, and Food Sensitivities
Gastrointestinal problems are common in children with ASD, especially chronic constipation, diarrhea, abdominal pain, and gastrointestinal inflammation [28,52]. A study by our group [53] found that those problems are strongly correlated to autism severity (r = 0.59, p < 0.001), suggesting that it is important to investigate them. As reported, in those with ASD, gastrointestinal problems appear to be partly due to deficiencies in digestive enzymes, partly due to food sensitivities, and possibly (as discussed above) due to low levels of omega-3 fatty acids, which in turn, could result in abnormal gut bacteria [54]. One large study by Horvath et al. evaluated disaccharidase activity from endoscopic biopsies in 90 children with ASD. They found that 49% had at least one deficient enzyme activity, and 20% had deficiencies in two or more disaccharidase enzymes “Lactase and maltase deficiencies were the most frequent, followed by low activity of sucrase, palatinase, and glucoamylase. All of the children with low enzyme activity had loose stools and/or gaseousness”. Another large study [55] involving intestinal biopsy samples of 199 children and adults with ASD (ages 22 months to 28 years) found that many had deficiencies in disaccharidases (enzymes for digesting simple sugars). Specifically, they found that 62% had deficiencies in lactase, 16% were deficient in sucrase, and 10% were deficient in maltase. The problems seemed to be equally common in children and adults, suggesting that these problems are lifelong. An open-label treatment study of 46 children and adults with ASD reported a wide range of benefits from the use of digestive enzymes [56], but results of randomized controlled trials are mixed [57,58]. Some studies have suggested that children with ASD have poor diets, leading to decreased intake of key nutrients [59,60].
Several studies have found that children with ASD have abnormal immune responses to certain foods, especially glutens (in wheat, rye, barley, oats) and casein (in dairy products) and sometimes soy. One study [61] found that many children with ASD have food sensitivities. Four studies [62,63,64,65] found that children with ASD had more hypersensitivities to food allergens than did typical children, and may be related to increased intestinal permeability [65,66]. A large study of 150 children with ASD found that 87% had IgG antibodies (sensitivity) to gluten, vs. 1% of the age and gender-matched controls, and 90% had IgG antibodies to casein, vs. 7% of the controls [67].
Several studies suggest that special diets can be beneficial for individuals with ASD. One open-label study [68] found that an 8-week diet which avoided allergic foods resulted in benefits in an open study of 36 children with ASD. One long-term open-label study of 70 children with ASD who followed a gluten-free, casein-free diet for one year or longer found that 81% improved significantly by the third month, with improvements continuing over the next 12 months. Large improvements were observed in social isolation, eye contact, mutism, learning skills, hyperactivity, stereotypic activity, and panic attacks [67]. A single-blind study of 10 children with autism found that 8 benefitted from a gluten-free, casein-free (GFCF) diet [69]. A 12-week, double-blind, cross-over study of a GFCF diet in 15 children with ASD did not find significant benefits, but parents reported benefits that were not identified by the testing [70]. However, a 12-month, randomized, single-blind, placebo-controlled GFCF diet study involving 54 children with ASD found statistically significant benefits in communication subscores (Autism Diagnostic Observation Schedule (ADOS) evaluation) in the GFCF diet group compared to the control group [71]. The parents (who were not blinded) also reported benefits in social interaction, daily living skills, inattention, and hyperactivity.
Overall, these studies suggest that children with ASD often have deficiencies in lactase and other digestive enzymes, may have poor diets, often have food sensitivities, especially to gluten and casein, and hence may benefit from digestive enzymes, healthier diets, and/or gluten-free, casein-free diets [65,66].
1.6. Study Goal
The goal of this study is to investigate a comprehensive nutritional and dietary intervention to treat children and adults with ASD. Each of these treatments have been previously studied individually and found to have some benefit, mostly in short-term studies. The goal of this study is to investigate the effect of the combination of those treatments in a long-term study. Combinations of these treatments are commonly used for treating children and adults with ASD, their effects are expected to be synergistic, and longer-term treatment may lead to greater benefits. An unusually wide age range was used in this study because this study was funded primarily by families participating in our annual walk fundraiser, and they have requested treatment studies that address all ages. This study is not designed to look at the effect of individual treatments (most of them have already been investigated individually); rather the goal is to investigate the effect of a combination of treatments which provide comprehensive, synergistic nutritional support.
1.7. Hypothesis
A combination of nutritional and dietary interventions will be effective in reducing the symptoms of autism, reducing gastrointestinal problems, and increasing overall functioning level.